Steve Franck’s Story
How a Medicare Coding Error Stopped Him from Getting the Medical Care He Needed
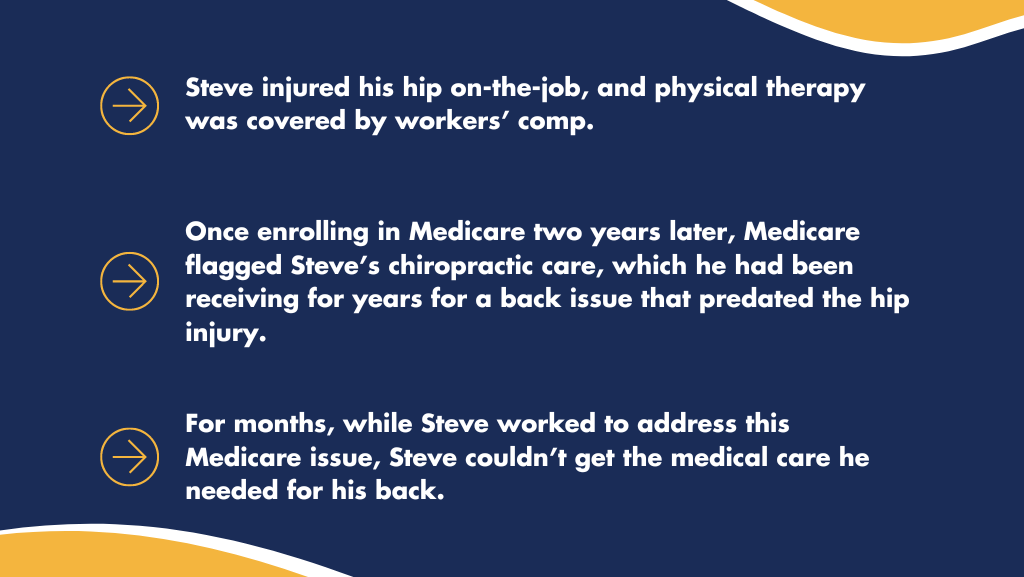
For many years I worked at a company that built tractor supplies, and my job required a lot of physical labor. I was constantly in motion, pulling parts on and off the products. One day, in November 2017, I was pulling a large part off some outdoor equipment and hurt my hip. At the time, I didn’t think it was that big of a deal, but it required medical attention, nonetheless. And, because my hip injury occurred while at work, my physical therapy was covered by workers’ compensation. After the recommended physical therapy, I resumed normal activity, and my hip was just fine.
Two years later, in 2019, I turned 65 and enrolled in Medicare.
Long before the workplace hip injury, an ongoing back issue sent me to a chiropractor. My back injury was a completely separate issue and happened many years before the 2017 incident. So, as I had for many years, I continued seeing my chiropractor for the ongoing back issue. Suddenly, they said they could not treat me due to an issue flagged through the Medicare system. Medicare had indicated they would not pay for the chiropractor or any type of medical care for my back injury, noting it should be covered by workers’ comp.
This didn’t make sense, since my back problem had predated the on-the-job hip injury that now was resolved, and I hadn’t had any coverage issues in the past.
The only thing that had changed was that I was now on Medicare.
I tried everything I could think of to get the issue with Medicare resolved. But at the end of the day, a simple coding error is what prevented me from getting the chiropractic care I needed for my back for entirely too long, jeopardizing my health and well-being. It took months going without treatment until one of the adjusters involved in my workers’ comp coverage was able to convince Medicare that the Medicare Secondary Payer laws did not apply, and that Medicare was responsible for my recurring back treatment.
This shouldn’t have happened to me, and it shouldn’t happen to others. Yet, it happens all the time—and it puts our health at risk. Medicare needs to update their process so that they can serve their beneficiaries, as intended.
The unfortunate issue Steve faced with Medicare confusing two separate claims is all too common among Medicare beneficiaries across the country.
Your stories matter. If you have a story similar to Steve’s and are willing to share, please contact the MARC Coalition so we can help advocate for change!